Multiple personality disorder had been used until 1994 and the idea was that there was additional information with these personalities, with these alters. So in a sense these alters were growing they were developing as individuals. In 1994 name is changed to Dissociative identity disorder (DID). With DID our understanding is that these alters are actually fragments of the original personality and no new information is being added, rather each alter represents a part of that personality. Dissociative identity disorder (DID) has the feature of alters or distinct personality states and this is the area that draws the controversy. This disorder had been sensationalized in the media, in movies and television. Other dissociative disorders are recognized by clinicians. All dissociative disorders mostly, but not necessarily, stem from severe childhood abuse and at the time of the abuse, the brain is trying to cope with the stress of the trauma, and it separates the individual from the reality. It causes dissociation and this dissociation is protective. It helps somebody to cope with these terrible traumatic events, but later in life individuals with dissociative disorders feel distress and need help.
In order to explain Dissociative identity disorder, first we must understand dissociative disorders.
What are dissociative disorders?
There are five dissociative disorders: Dissociative identity disorder (DID), Dissociative amnesia including Dissociative Fugue, Depersonalization/Derealization disorder, Other Specified Dissociative Disorder and Unspecified Dissociative Disorder. Dissociative identity disorder will be explained last.
Dr. Marlene Steinberg, who developed the Structured Clinical Interview for Dissociative Disorders to assess dissociation, analyzed the characteristics of dissociative disorders, finding that each dissociative disorder could be described and understood using a combination of one of five core symptoms: The Five Core Components of Dissociative Disorders.
Amnesia – recurrent memory problems, often described as “losing time”, these gaps in memory can vary from several minutes to years
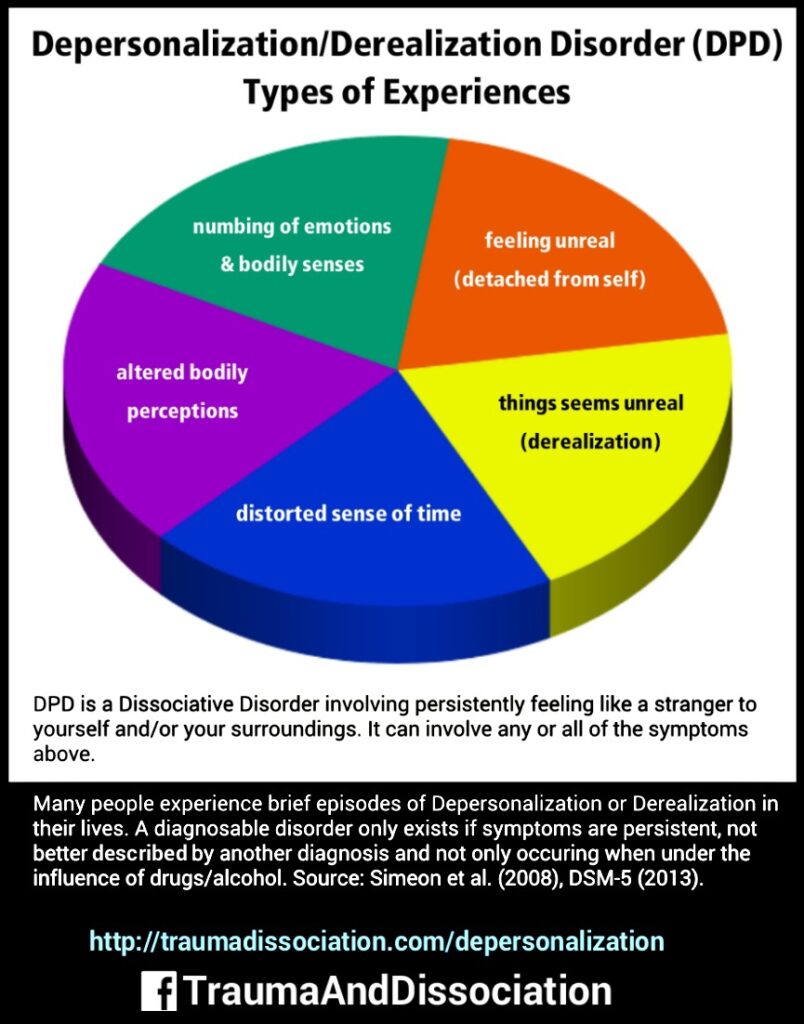
Depersonalization – a sense of detachment or disconnection from one’s self, this can include feeling like a stranger to yourself, feeling detached from your emotions, feeling robotic or like you are on autopilot, or feeling like a part of your body does not belong to you. Some people self-injure when depersonalized, for example in order to feel “real”.
Derealization – a sense of disconnection from familiar people or one’s surroundings, for example, close relatives or your own home may seem unreal or foreign. Episodes of derealization may happen during flashbacks; you may suddenly feel much younger and feel your present environment is unreal during this time.
Identity confusion – an inner struggle about one’s sense of self/identity, which may involve uncertainty, puzzlement or conflict. Severe identity confusion regarding sexual identity has been reported in people who have been sexually abused.
Identity alteration – a sense of acting like a different person some of the time. Recognizable signs of identity alteration include using of different names in different situations, discovering you have items you don’t recognize, or having a learned skill which you have no recollection of learning. Mild identity alteration is widespread in the non-clinical population and does not cause difficulties for the person, for example a person assumes different roles but remained aware of this alteration. Mood or behavior changes which don’t feel under your control, but don’t involve using different names or changes in memory or perceived age, etc., indicate moderate identity alteration. This is common in non-dissociative disorders, for example in borderline personality disorder.
Traumadissociation.com (Aug 17, 2024). Dissociative Disorders. Retrieved Aug 17, 2024 from
http://traumadissociation.com/dissociative.html
- Dissociative identity disorder
- Dissociative amnesia, including Dissociative Fugue
Dissociative amnesia is the most common Dissociative Disorder. There are several different types of amnesia, and many different causes. Dissociative Amnesia is not caused by head injuries or physical damage to the brain, it is amnesia which has a psychological cause. It can occur as part of a number of other mental health conditions, including posttraumatic stress disorder and acute stress disorder, dissociative identity disorder, somatoform disorder and anxiety disorders. In any of those cases it would not be classed as a separate disorder. Dissociation Amnesia can last for between a few days to a few years, but is typically less than a week. The period of time which cannot be remembered can range from minutes to decades. The DSM-5 states that the key characteristic is “the inability to recall important autobiographical information that: should be successfully stored in memory and ordinarily would be readily remembered (Criteria A).”
Because there is no neurobiological damage or toxicity, and the difficulties are in retrieving a memory which was successfully stored, the amnesia is always “potentially reversible”. Neurocognitive disorders involving memory loss usually include cognitive (thinking) and intellectual impairments in memory, these are not present in people with Dissociative Amnesia. Dissociative amnesia is more likely in people with a history of multiple adverse childhood experiences (especially if they include physical or sexual abuse), people who have experienced interpersonal violence (for example, domestic violence or physical assaults), and the risk increases with the “severity, frequency, and violence of the trauma”.
The three common types of dissociative amnesia are localized amnesia, selective amnesia (which may occur along with localized amnesia), and generalized amnesia.
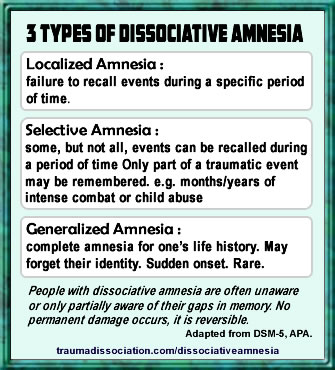
Generalized amnesia may involve the complete loss of a person’s identity, in addition to all memories of their past. Other forms of dissociative amnesia can also occur; people with generalized amnesia (the most severe type) may also lose semantic knowledge (previous knowledge about the world) and procedural knowledge (forgetting well-learned skills). Systematized amnesia is amnesia for a category of information (e.g., no memory of family, no memory of a specific person, or childhood sexual abuse). Continuous amnesia is unable to form new memories. Micro-amnesias are also typical in dissociative disorders, the amnesia is for very, very brief periods of time. The International Society for the Study of Trauma and Dissociation gives the example of forgetting the contents of a conversation from one moment to the next. The person may struggle to work out what was discussed while trying to avoid the other person realizing this. Dissociative Amnesia has been previously known as Psychogenic Amnesia, and Hysterical Amnesia.
The newly released guide to diagnosing mental disorders is the DSM-5, released in 2013, gives the following diagnostic criteria: “A. An inability to recall important autobiographic information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting. Note: Dissociative Amnesia most often consists of localized or selective amnesia for a specific event or events; or generalized amnesia for identity and life history. B. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. C. The disturbance is not attributable to the physiological effects of a substance (e.g., alcohol or other drug abuse, a medication) or a neurological or other medical condition (e.g., partial complex seizures, transient global amnesia, sequelae of a closed head injury/traumatic brain injury, other neurological condition). D. The disturbance is not better explained by dissociative identity disorder, posttraumatic stress disorder, acute stress disorder, somatic symptom disorder, or major or mild neurocognitive disorder.”
Specify if: “With dissociative fugue: Apparently purposeful travel or bewildered wandering that is associated with amnesia for identity or other important autobiographical information.”
During a Dissociative Amnesia with Fugue, a person normally acts in a way which is purposeful and has a specific goal; fugue states may last for days, weeks, or longer. A fugue occurs when there is sudden and unexpected travel away from home or work in combination with amnesia for a person’s past, and either identity confusion or assumption of a new identity. Dissociative Fugue is also known as Psychogenic Fugue, and was previously a separate diagnosis, but is combined with Dissociative Amnesia in the DSM-5. It can be distinguished from amnesia and the aimless wandering sometimes present during seizures using tests such as EEGs to establish if there is a relationship between seizure activity and the amnesia.
Dissociative Amnesia & Fugue. (Aug 17, 2024). Traumadissociation.com, Retrieved Aug 17, 2024 from http://traumadissociation.com/dissociativeamnesia.html
- Depersonalization/Derealization disorder
Depersonalization/Derealization Disorder is a Dissociative Disorder.
Many people with this disorder have a history of childhood trauma, particularly emotional abuse and emotional neglect. Other known factors include witnessing domestic violence, by raised by a parent with serious mental illness or the sudden death or suicide of a relative or close friend. The average age of onset is 16, and 95% of people have symptoms prior to the age of 25. Another known cause of this disorder is recreational drug use (substance use), especially Marijuana, ecstasy and Ketamine (Special K). Depersonalization/Derealization disorder caused by drug use cannot be cured by stopping using the drug that caused it, this is because the disorder can only be diagnosed if symptoms continue after stopping using the drug. Marijuana (cannabis) use may occur prior to new panic attacks and depersonalization/derealization symptoms.
http://traumadissociation.com/depersonalization
According to the DSM-5: “A. The presence of persistent or recurrent experiences of depersonalization, derealization or both: Depersonalization: Experiences of unreality, detachment, or being an outside observer with respect to one’s thoughts, feelings, sensations, body, or actions (e.g., perceptual alterations, distorted sense of time, unreal or absent self, emotional and/or physical numbing). Derealization: Experiences of unreality or detachment with respect to surroundings (e.g., individuals or objects are experienced as unreal, dreamlike, foggy, lifeless, or visually distorted). B. During the depersonalization or derealization experiences, reality testing remains intact. C. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. D. The disturbance is not attributable to the physiological effects of a substance (e.g., a drug of abuse, medication) or other medical condition (e.g., seizures). E. The disturbance is not better explained by another mental disorder, such as schizophrenia, panic disorder, major depressive disorder, acute stress disorder, posttraumatic stress disorder or another dissociative disorder.”
The conditions below may cause a person to describe symptoms similar to Depersonalization/Derealization disorder.
- Illness anxiety disorder, for example, if there are vague physical complaints or fears of permanent brain damage.
- Major depressive disorder, if only numbness, deadness and apathy occur.
- Obsessive-compulsive disorder, if there is obsessive checking of symptoms or rituals.
- Other dissociative disorders such as Dissociative Identity Disorder, Dissociative Amnesia and Conversion Disorder (Functional Neurological Symptom Disorder). If Dissociative Identity Disorder (DID) is present Depersonalization/Derealization disorder should not be diagnosed in addition because these experiences are also known to occur within DID.
- Anxiety disorders, e.g. panic disorder, social anxiety disorder, or specific phobia may be diagnosed if symptoms only occur during a panic attack.
- Psychotic disorders, delusions or results from reality testing can confirm a psychotic disorder, for example a Delusional Disorder or Schizophrenia, may cause a person to believe they are dead or the world no longer exists.
- Substance or medication-induced disorders, Depersonalization/derealization disorder can be caused by acute use of, or withdrawal from, Marijuana (cannabis), hallucinogens (e.g., LSD, magic mushrooms, mescaline), ketamine, MDMA/ecstasy, and salvia but should not be diagnosed unless symptoms continue for some time after the substance use ends.
- Mental disorders due to another medical condition, e.g. temporal lope epilepsy, or partial and frontal lobe epilepsy. Depersonalization/Derealization Disorder. (Aug 17, 2024). Traumadissociation.com. Retrieved Aug 17, 2024 from http://traumadissociation.com/depersonalization.html
- Other Specified Dissociative Disorder
DSM-5 Diagnostic Criteria: “This category applies to presentations in which symptoms characteristic of a dissociative disorder that cause clinically significant distress or impairment in social, occupational, or other important areas of functioning predominate but do not meet the full criteria for any of the disorders in the dissociative disorders diagnostic class. The other specified dissociative disorder category is used in situations in which the clinician chooses to specify reason that the presentation does not meet the criteria for any specific dissociative disorder. This is done by recording “other specified dissociative disorder” followed by the specific reason (e.g., “dissociative trance”). Example presentations that can be specified using the “other specified” designation include the following: “1. Chronic and recurrent syndromes of mixed dissociative symptoms. This category includes identity disturbance associated with less than marked discontinuities in sense of self and agency, or alterations of identity or episodes of possession in an individual who reports no dissociative amnesia. 2. Identity disturbance due to prolonged and intense coercive persuasion: Individuals who have been subjected to intense coercive persuasion (e.g., brainwashing, thought reform, indoctrination while captive, torture, long-term political imprisonment, recruitment by sects/cults or by terror organizations) may present with prolonged changes in, or conscious questions of, their identity. 3. Acute dissociative reactions to stressful events: This category is for acute, transient conditions that typically last less than 1 month, and sometimes only a few hours or days. These conditions are characterized by constriction of consciousness; depersonalization; derealization; perceptual disturbances (e.g., time slowing, macropsia); micro-amnesias; transient stupor; and/or alterations in sensory-motor functioning (e.g., analgesia, paralysis). 4. Dissociative trance: This condition is characterized by an acute narrowing or complete loss of awareness of immediate surroundings that manifest as profound unresponsiveness or insensitivity to environmental stimuli. May be accompanied by minor stereotyped behaviors of which the individual is unaware and/or that he or she cannot control, as well as transient paralysis or loss of consciousness. The dissociative trance is not a normal part of a broadly accepted collective cultural or religious practice. “
Other Specified Dissociative Disorder. Traumadissociation.com. (Aug 17, 2024). Traumadissociation.com. Retrieved Aug 17, 2024 from http://traumadissociation.com/osdd.htmlhttp://traumadissociation.com/osdd.html
- Unspecified Dissociative Disorder
Unspecified Dissociative Disorder DSM-5 Diagnostic Criteria: “This category applies to presentations in which symptoms characteristic of a dissociative disorder that cause clinically significant distress or impairment in social, occupational, or other important areas of functioning predominate but do not meet the full criteria for any of the disorders in the dissociative disorders diagnostic class. The unspecified dissociative disorder category is used in situations in which the clinician chooses not to specify the reason that the criteria are not met for a specific dissociative disorder, and includes presentations for which there is insufficient information to make a more specific diagnosis (e.g., in emergency room settings). ” This diagnosis, along with Other Specified Dissociative Disorder, act as a “residual category for dissociative symptoms which do not fit within a more specific category” and either the clinician decides not to specify the reason that the criteria for other Dissociative Disorders aren’t met, or not information exists to make a more specific diagnosis. As described above, there must be clinically significant impairment or impaired functioning as a result of the dissociative symptoms. Unspecified Dissociative Disorder. (Aug 17, 2024). Traumadissociation.com. Retrieved Aug 17, 2024 from http://traumadissociation.com/udd.html
What is Dissociative Identity Disorder? DID is: a psychobiological response to traumas suffered in a specific time window in early childhood, a dissociative disorder and a complex posttraumatic stress syndrome. How does DID develop? An important step in childhood development – the formation of a central, integrated consciousness – is impeded or prevented by repeated trauma. The child uses radical denial and splitting to cope with the traumas, imagining that the traumas happened to “someone else”. The child’s fantasy capabilities and imagination give the different personality states their individual characteristics. The extremely inconsistent and contradictory behavior of attachment figures and their denial of the trauma suffered by the child additionally foster the dissociative coping strategy.
Dissociative Identity Disorder is caused by “overwhelming experiences, traumatic events, and/or abuse occurring in childhood”, particularly when repeated traumas begin before age 5 or 6. The child’s repeated, overwhelming experiences usually occur alongside a disturbed or disrupted attachment style between the parent/caregiver and the child. Dissociative Identity Disorder is often, but not always, caused by early child abuse (including neglect and the failure to respond to the child). Other early and chronic traumatization can cause it, e.g., medical trauma, involving multiple painful and prolonged medical procedures at an early age. Early childhood trauma causes Dissociative Identity Disorder to develop by preventing the child from forming a cohesive and fully integrated or unified sense of self, known as a core or fully integrated personality, during their earliest years. Instead of integrating into a core personality, people with DID experience prolonged trauma in early childhood which causes the original different “behavioral states” present from birth to become parts of the personality that are increasingly dissociated (disconnected) from each other, which prevents them from integrating to form a core personality. Over time, the early dissociated behavioral states, influenced by the trauma, develop into dissociative identities (also known as dissociative personality states, distinct personality states, alternate identities or alters). It is generally accepted that developing multiple identities protects the child psychologically by keeping trauma memories and emotions contained with specific identities, rather than overwhelming the child completely.
The DSM-5 gives the following diagnostic criteria for Dissociative Identity Disorder: “A. Disruption of identity characterized by two or more distinct personality states, which may be described in some cultures as an experience of possession. The disruption of marked discontinuity in sense of self and sense of agency, accompanied by related alterations in affect, behavior, consciousness, memory, perception, cognition, and/or sensory-motor functioning. These signs and symptoms may be observed by others or reported by the individual. B. Recurrent gaps in the recall of everyday events, important personal information, and/or traumatic events that are inconsistent with ordinary forgetting. C. The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. D. The disturbance is not a normal part of a broadly accepted cultural or religious practice. Note: In children, the symptoms are not better explained by imaginary playmates or other fantasy play. E. The symptoms are not attributable to the physiological effects of a substance (e.g., blackouts or chaotic behavior during alcohol intoxication) or another medical condition (e.g., complex partial seizures).” A mix of secondary symptoms are found in DID, particularly those caused by the passive influence of alters intruding into awareness, but no single secondary symptom is present in everyone with Dissociative Identity Disorder, and these do not form part of the diagnostic criteria.
The DSM 5 lists the following alternative diagnoses, which may be considered/ruled out during the Dissociative Identity Disorder diagnostic process. Any of these can be co-morbid with Dissociative Identity Disorder, except for Other Specified Dissociative Disorder.
- Other Specified Dissociative Disorder (formerly Dissociative Disorder Not Otherwise Specified) This can’t occur alongside DID because it is only diagnosed when someone does not quite meet the DID criteria. The two most common forms of Other Specified Dissociative Disorder involve having amnesia and dissociative parts of your personality which are not quite distinct/separate enough for DID, and having dissociative parts which are distinct enough to be alter personalities but without amnesia between them.
- Major Depressive Disorder (often just called “depression”). Depression is very common in people with DID, but both depressed mood and depressive thoughts fluctuate, because they are present in some alters but not others. Because of this, Other specified depressive disorder may be diagnosed along with DID.
- Bipolar Disorders – especially Bipolar II. Changes in mood occur in Dissociative Identity Disorder due to switching between alters (alters often have different mood states to each other). Bipolar II does not involve full-blown mania.
- Posttraumatic Stress Disorder – There is now a dissociative subtype of PTSD and some overlapping features between DID and PTSD. PTSD is commonly comorbid with DID, but key differences exist as well. Complex PTSD is diagnosed as just PTSD in the DSM-5 (it is not considered a separate disorder). Differences between DID and Complex PTSD are described in the Dissociative Identity Disorder treatment guidelines for Adults; Complex PTSD is very common in people with Dissociative Identity Disorder, and dissociation is a symptom of both.
- Psychotic Disorders (including Schizophrenia) – Hearing voices (which come from alter personalities), and symptoms of partial flashbacks like feeling touched when nobody is there may be mistaken for psychotic hallucinations. The passive influence of alters causes many psychotic-like symptoms, but without any loss of contact with reality.
- Personality Disorders (especially Borderline Personality Disorder(BPD). BPD has both transient stress-related dissociative symptoms and identity disturbance within its diagnostic criteria. Psychological tests can be used to determine if Dissociative Identity Disorder is present, and whether a personality disorder is also present. Self-injury and self-destructive behavior is also common in both DID and BPD.
- Substance/medication-induced disorders (e.g., alcohol or drug addiction or side effects of another drug). Certain substances can cause episodes of amnesia and altered behavior (e.g. alcohol) or other dissociative experiences – in DID these occur during times when no substance has been used. Substance use disorders are common in people with DID.
- Conversion Disorder (Functional Neurological Symptom Disorder). These disorders are common in people with DID, particularly psychogenic non-epileptic seizures (PNES), which can cause amnesia during the seizure only.
- Seizure Disorders – especially Complex Partial Seizures. EEG tests can differentiate between seizure disorders and seizure-like symptoms in DID. Dissociative symptoms are far greater in people with DID.
- Factitious Disorder and Malingering Both of which involve intentionally and knowingly pretending to have DID, e.g. by repeatedly giving false information to professionals. This is very different to having doubts about symptoms, or wondering if you ‘made it all up’. Psychological tests, observation, and corroborating history can be used to help diagnose. Malingerers have a clear motive, e.g. to avoid responsibility for a crime (despite the fact the diagnosis is rarely accepted for an ‘insanity’ defense).
A change introduced in the DSM-5 makes it possible to diagnose DID without the diagnosing clinician directly observing a switch between alters: instead, DID can be diagnosed if the person self-reports their presence and effects, or if another person describes observing a switch between alters. Two clusters of symptoms indicate the presence of alters if they are not observed. These are described in the DSM-5’s extended description of Dissociative Identity Disorder: Sudden alterations or discontinuities in sense of self and sense of agency (Criteria A), and recurrent episodes of dissociative amnesia (Criteria B).
Sense of Self and Agency The terms “sense of self” and “sense of agency” are used in the DSM’s Dissociative Identity Disorder Criterion A, which describes the presence of distinct personality states, better known as alter personalities. It is the discontinuities (switches) between alters, as well as their presence, that this criterion describes. A discontinuity in a person’s sense of self can affect any part of someone’s functioning. Attitudes, outlooks and personal preferences like preferred foods or clothes may change suddenly and inexplicably, and then change back again. This happens because alter personalities have different attitudes, outlooks and preferences, so a very sudden change without explanation occurs when an alter has either taken control or is strongly influencing the person. When that alter is no longer active, everything changes back (until the next time the same alter is active). During these times, a person may find have bought clothes they would never choose to wear, or a very outgoing person may suddenly become shy and introverted with no apparent reason. Discontinuity in a person’s sense of agency means not feeling in control of, or as if you don’t “own” your feelings, thoughts or actions. For example, experiencing thoughts, feelings or actions that seem as if they are “not mine” or belong to someone else. This is not the delusional belief that they belong to an outside person, it is the perception that their own speech, thoughts, and/or behavior do not feel like they belong to them and may make no sense to them. Emotions and impulses are often described as puzzling to the person. This happens in Dissociative Identity Disorder because some of the thoughts, feelings or actions of alter personalities intrude into their conscious awareness, even when they are not aware they have any alter personalities, or have amnesia for their actions. This is known as passive influence or partially dissociated intrusions of alter identities into conscious awareness. A person with DID may also experience a fully dissociated intrusion.
A similar depersonalized experience can happen briefly during times of severe stress, especially in people with Borderline Personality Disorder, except that the person perceives the behavior as “out of character” rather than like being a totally different person. In Dissociative Identity Disorder, there may no obvious stressor or trigger causing the switch in personality state, the actions and words spoken may not relate to any prior distress, and the duration can be considerably longer (hours, days, or more). In DID, this happens because an alter personality has taken executive control, so attitudes, outlook and personal preferences change at the same time – leaving a feeling as if someone else is in control of their body. This change in control is known as switching, only in Dissociative Identity Disorder or similar forms of Other Specified Dissociative Disorder can a person switch to an alter personality, because no other diagnosis has alter personalities that control (of the body) can be switched to. Rapidly switching moods (within minutes or hours) are commonly caused by the presence of alters which have different moods, these changes in moods can be puzzling and lead to a misdiagnosis of Bipolar Disorder, type 2, however mood changes in Bipolar Disorder do not switch back and forth as rapidly, with rapid-cycling bipolar involving several switches per year only.
The combined changes in “sense of self” and “sense of agency” can cause a person to find themselves feeling like they are watching passively while someone else controls their body; they hear themselves speaking words they would never normally speak and that may not make sense to them, and which they are powerless to stop. The person has become a depersonalized observer of themselves. Some people describe this combined change of “sense of self” and “sense of agency” as feeling like an experience of possession, in a non-religious sense, or having their body “hijacked”. A person with DID may find that their body feels totally different during this time (e.g., like a small child, the opposite gender, huge and muscular), or may feel as if they are suddenly younger or older.
In DID, total amnesia for the actions of alter personalities is not necessary – it is possible for a person to be aware of many of their actions at the time, known as co-consciousness, or remember some of what happened later. If a person does have total amnesia the changes in a person’s speech, mood and behavior may be witnessed by others and reported back to them, but they may deny this “odd behavior” because they have no memory of it, which can lead others to incorrectly assume they are repeatedly lying. Several different types of amnesia can occur in people with Dissociative Identity Disorder. The common types are:
“gaps in past memory of personal life events” (e.g., periods of childhood or adolescence; some important life events, such as the death of a grandparent, getting married, giving birth); this amnesia does not need to be restricted to traumatic events.
“lapses in dependable memory” (e.g., of what happened today, remembering how to do well-learned skills like how to do their job, drive, read, etc.); this refers to the whole person – for example having a child alter who does not know how to read would prevent the person from remembering how to read when that alter was in control of the body.
“discovery of evidence of their everyday actions and tasks that they do not recollect doing” (e.g., finding unexplained objects in their shopping bags or among their possessions; finding perplexing writings or drawings that they must have created; discovering injuries; “coming to” in the midst of doing something). Dissociative fugues, which involve travel to an unusual place without any memory of the journey or its purpose, are common. People find suddenly find themselves “coming to” at the beach, hiding in a closet at home, in a nightclub, or in bed without any memory of the “lost” time.
People with total amnesia for the actions of alter personalities may refer to the periods of amnesia as blackouts or losing time, and may not be aware that they have alter personalities, this degree of amnesia does occur in some people with DID but has never been a required diagnostic criterion. Other people with DID may have internal conversations with their alters and are able to describe them, which is something asked about in the Structured Clinical Interview for Dissociative Disorders. If no recurrent (reoccurring) gaps in memory for the past or present occur but all the other criteria are met, then the similar diagnosis of Other Specified Dissociative Disorder Presentation 1 can be given instead. The three common types amnesia found in DID can be assessed using diagnostic screening and/or a clinical interview for Dissociative Disorders.
Dissociative Identity Disorder. (Aug 17, 2024) Traumadissociation.com, Retrieved Aug 17, 2024 from http://traumadissociation.com/dissociativeidentitydisorder.html